Menu
Vein Occlusion
Central Retinal Vein Occlusion (CRVO)
Branch Retinal Vein Occlusion (BRVO)
What is Vein Occlusion?
Veins are the blood vessels that take blood away from the eye and towards the heart. Veins are present in the retina, which is home to the light sensing tissue at the back of the eye. Retinal vein occlusion occurs when there is a blockage of a retinal vein and this results in leaking and bleeding into the retina.
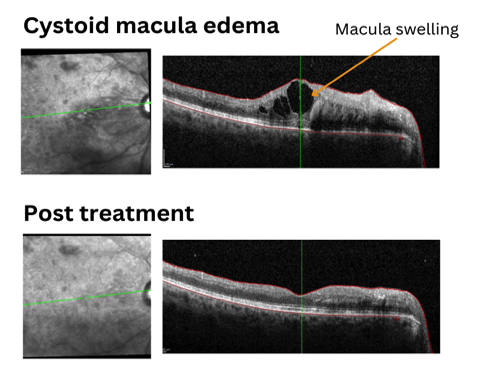
This swelling can disrupt vision particularly if the fluid accumulates in the macula, as the macula is responsible for central detailed vision. This is known as macular oedema. The blockage may occur in the central retinal vein or one of its branches.
What can I expect for my first intravitreal injection?
You will initially see an orthoptist who will review your history, check your vision and perform an initial eye exam. You will receive dilating eye drops that allow a complete retinal exam which can blur your vision over the next few hours and cause light sensitivity. You will have a scan of your retina performed (OCT) which provides images of the macula and layers of the retina.
You will then see your treating doctor for further eye examination and discussion of your disease. You will have the chance to discuss the risks and learn about how the treatment will work within the eye. You can also ask any questions you might have and learn what you might expect after the injection.
The injection will be performed with prior antiseptic (cleaning) and anaesthetic (numbing) for your comfort. You will be given instructions to keep the eye clean post-injection and you should arrange a safe way to get home as you should avoid driving home directly after your appointment. Return to Top
- Side effects of intravitreal injections
Common side effects include irritation, small number of floaters and some redness around the injection area. Symptoms of concern include worsening vision, multiple floaters, achey pain and flashing lights.
- Complications are rare but serious complications may include endophthalmitis (infection of the inside of the eye) which has an incidence rate of 0.02%.[5] There is also a risk of increased intraocular pressure, vitreous haemorrhage and retinal tear/detachment
Laser Therapy
Laser treatment may be employed to resolve abnormal new blood vessel growth in certain cases.
Site by Constant Creations
Types of Vein Occlusion?
Central Retinal Vein Occlusion (CRVO)
This occurs when the main vein that drains blood from the entire retina becomes blocked. This can lead to bleeding (haemorrhaging) throughout the retina.
In some cases of central vein occlusion, blood flow may become so poor that tissues also become oxygen-starved. This is known as ischemia which can lead to the release of hormones that trigger new blood vessel growth, for example, VEGF or vascular endothelial growth factor.
VEGF can cause growth of new, abnormal vessels which are particularly leaky and also make normal blood vessels leaky. Ischemic CRVO causes worse vision outcomes and poorer chance of recovery of vision.
Branch Retinal Vein Occlusion (BRVO)
In this type, one of the smaller branch veins that supply blood to a particular part of the retina is blocked. Haemorrhaging will be less extensive than CRVO and restricted to a smaller area. However, the macula may still be affected and cause disturbance to central vision depending on the vessel affected.
BRVO is more common than CRVO. Prognosis is better in BRVO than CRVO. Patients with BRVO will often have good recovery of vision, with 50-60% of untreated BRVO cases having recovery of vision to the line required for driving standards in that eye.[1]
Causes of Vein Occlusion
Risk factors for retinal vein occlusion include:
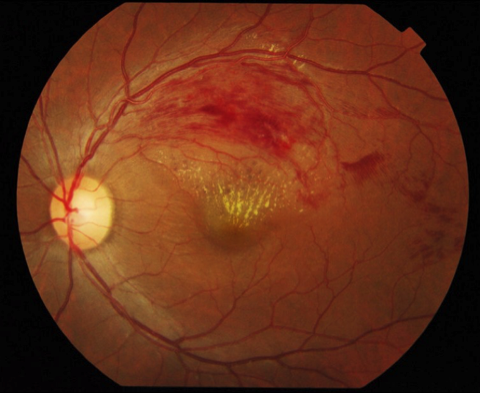
Branch retinal vein occlusion image by Ku C Yong, Tan A Kah, Yeap T Ghee, Lim C Siang and Mae-Lynn C Bastion, Department of Ophthalmology, Universiti Kebangsaan Malaysia Medical Centre (UKMMC) and Universiti Malaysia Sarawak (UNIMAS), Kuala Lumpur, Malaysia. Licensed under CC BY 2.0.
References
1. Ocular vascular occlusive disorders: Natural history of visual outcome. In Progress in Retinal and Eye Research Vol. 41, Issue 1, pp. 1–25.Hayreh, S. S. (2014). Elsevier Ltd.
2. Traditional and novel cardiovascular risk factors for retinal vein occlusion: The multiethnic study of atherosclerosis. Investigative Ophthalmology and Visual Science, 49(10), 4297–4302. Cheung, N., Klein, R., Jie, J. W., Cotch, M. F., Islam, A. F. M., Klein, B. E. K., Cushman, M., & Tien, Y. W. (2008).
3. Ranibizumab for Macular Edema following Central Retinal Vein Occlusion. Six-Month Primary End Point Results of a Phase III Study. Ophthalmology, 117(6). Brown, D. M., Campochiaro, P. A., Singh, R. P., Li, Z., Gray, S., Saroj, N., Rundle, A. C., Rubio, R. G., & Murahashi, W. Y. (2010).
4. Ranibizumab for Macular Edema following Branch Retinal Vein Occlusion. Six-Month Primary End Point Results of a Phase III Study. Ophthalmology, 117(6). Campochiaro, P. A., Heier, J. S., Feiner, L., Gray, S., Saroj, N., Rundle, A. C., Murahashi, W. Y., & Rubio, R. G. (2010).
5. Issues with intravitreal administration of anti-vegf drugs. Clinical Ophthalmology, 14, 897–904. Schargus, M., & Frings, A. (2020).
Managing Vein Occlusion
Anti-VEGF Injections
Intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) medications can help reduce swelling and improve visual outcomes. Anti-VEGF is particularly used in cases of macular oedema, when swelling and bleeding has occurred in the macula which provides central vision.
Anti-VEGF has been shown to improve vision in both BRVO and CRVO patients. In both groups, studies have shown an average improvement of approximately 3 lines after 6 months, compared to a 1 line improvement in vision in untreated BRVO, and no improvement in the CRVO group over the same time.[3] [4].

