Menu
Age Related Macular Degeneration (AMD)
What is Age Related Macular Degeneration?
Early-Intermediate AMD
Advanced AMD
Novel treatments
Intravitreal injections
What to expect for your first IV injection
What is Age Related Macular Degeneration?
Age related Macular Degeneration(AMD) is a common eye condition that affects people over 50 through changes and damage to the macula. The macula is an area of the retina which is responsible for central vision which allows you to see fine details clearly and perform activities such as reading and driving.
AMD is the most common cause of reduced vision in older people in the developed world. In 2010 AMD was responsible for vision impairment in 107,000 Australians.[1]
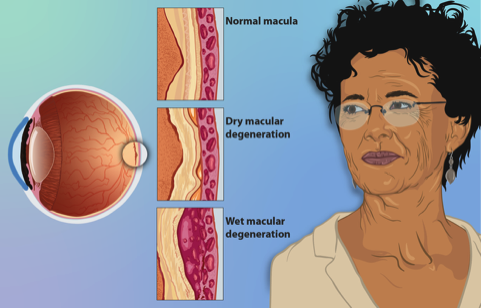
Regular eye checks can detect changes associated with AMD as early stages of the disease may not cause obvious visual symptoms.[2] Macular degeneration is often divided into wet and dry types and treatment options for both are receiving ongoing research.
Early-Intermediate AMD
The macula contains some of the most metabolically active cells in the entire body, because photoreceptor (light-sensing cells in the retina) shed their tips on a daily basis.
These waste products are metabolised by the outer retina in a layer known as the retinal pigment epithelium, which also is involved in other processes important to our vision.
Over time, incompletely processed waste builds up and can be a focus of inflammation. All early and intermediate AMD is considered ‘dry’.
Advanced AMD
Advanced AMD can be either dry or wet.
Advanced Dry AMD occurs when the outer retina layers (RPE and photoreceptors) are lost (atrophy) resulting in small bare patches in the retina, like worn out carpet. These patches are non-functional, causing missing patches in the vision. Vision loss can be severe in advanced dry AMD, also known as atrophic AMD, if the very centre of the vision is involved.
Wet Macular Degeneration (Neovascular AMD): occurs when abnormal blood vessels grow under and into the retina as a response to inflammation, leaking blood, fluid and causing scarring. The fluid and blood leakage can disturb the layers of the macula and cause rapid central vision changes and loss. Wet AMD should be frequently monitored by an ophthalmologist who may consider treatment options, such as intravitreal injection of medication, to reduce blood vessel growth.
Types of Macular Degeneration
Causes of AMD
Age: Macular degeneration is primarily age-related, usually affecting people over 50 years old. Risk of developing AMD increases with age.[3]
Genetics: A family history of macular degeneration increases the risk.
Smoking: Smoking significantly increases the risk of developing AMD
Hypertension: High blood pressure can contribute to macular degeneration.
Diet: A poor diet lacking in nutrients, especially antioxidants and zinc, can be a risk factor.
Symptoms
Blurred vision: You may notice increased difficulty reading or recognising faces.
Distorted Vision: Straight lines may appear wavy or bent.
Dark or Empty patches in vision: Missing patches in vision may develop in advanced disease.
Muted colours: You may notice changes to your colour vision, as the macula is the home of many of the receptors needed for good colour vision.
Prevention
Healthy Lifestyle: Maintain a balanced + colourful diet. Incorporate leafy greens and foods high in zinc + antioxidants such as nuts, fruits and vegetables. Keep up regular exercise that increases your heart rate such as walking, swimming and pilates.
Supplements: Your ophthalmologist may suggest supplements to be used in conjunction with a healthy diet.
Protect Your Eyes: Wear sunglasses that block harmful UV rays.
Avoid smoking and reduce alcohol intake.
Regular Eye Check-ups: Early detection through regular eye exams is crucial. Your doctor may provide you a grid known as an Amsler Grid to regularly check for changes in your vision one eye at the time. Regularly checking your grid is important to alert us of changes to the macula that you might not notice otherwise.
Treatments
Novel treatments
Until recently, there has been no treatment for atrophic (dry) AMD, but a new class of drugs which inhibit part of the body's innate immune system, known as the complement cascade, have returned early positive results in reducing atrophy in Phase 3 studies. The first two drugs of this class are available in the USA and are likely to be available in Australia in the next 12 months. They are incompletely effective in that they slow, not stop, the progression of the thinning but do not reverse damage.[4]
Intravitreal injections
The most frequently prescribed treatments for wet AMD are delivered through intravitreal injections. These medications block the activity of hormones such as VEGF (Vascular endothelial growth factor A) and more recently, Angiopoietin-2. These hormones are responsible for triggering the growth of blood vessels in the eye and are typically abnormally high in people with wet AMD. Regular treatment with these intravitreal injections can reduce blood vessel growth and the associated leakage and swelling in the macula.
Studies show the average result of regular intravitreal injections for AMD is a 1-2 line improvement in vision, and 34-41% of people experience a 3 line or more improvement in their vision.[5]
What can I expect for my first intravitreal injection?
You will initially see an orthoptist who will review your history, check your vision and perform an initial eye exam. You will receive dilating eye drops that allow a complete retinal exam which can blur your vision over the next few hours and cause light sensitivity. You will have a scan of your retina performed (OCT) which provides images of the macula and layers of the retina.
You will then see your treating doctor for further eye examination and discussion of your disease. You will have the chance to discuss the risks and learn about how the treatment will work within the eye. You can also ask any questions you might have and learn what you might expect after the injection.
The injection will be performed with prior antiseptic (cleaning) and anaesthetic (numbing) for your comfort. You will be given instructions to keep the eye clean post injection and you should have a safe way to get home as you should avoid driving home directly from your appointment.
Side effects - The most common side effects include irritation, small number of floaters and some redness around the injection area. Symptoms of concern include worsening vision, multiple floaters, achey pain and flashing lights.
Complications - are rare but can be serious. Complications include endophthalmitis (infection of the inside of the eye) which has an incidence rate of 0.02%.[6] There is also a risk of increased intraocular pressure, vitreous haemorrhage and retinal tear/detachment.
References
[1] Deloitte Access Economics, & Mitchell, P. (2011). Eyes on the future: A clear outlook on Age-related Macular Degeneration. Macular Disease Foundation Australia.
[2] Mitchell, P., Liew, G., Gopinath, B., & Wong, T. Y. (2018). Age-related macular degeneration. Lancet, 392, 1147–1159
[3] Smith, W., Assink, J., Klein, R., Mitchell, P., Klaver, C. C. W., Klein, B. E. K., Hofman, A., Jensen, S., Wang, J. J., & de Jong, P. T. V. M. (2001). Risk Factors for Age-related Macular Degeneration Pooled Findings from Three Continents. Ophthalmology, 108 (4)(697–704).
[4] Spaide, R. F., & Vavvas, D. G. (2023). COMPLEMENT INHIBITION FOR GEOGRAPHIC ATROPHY Review of Salient Functional Outcomes and Perspective. Retina, 43(7), 1064–1069.
[5] Brown, D. M., Michels, M., Kaiser, P. K., Heier, J. S., Sy, J. P., & Ianchulev, T. (2006). Ranibizumab versus Verteporfin Photodynamic Therapy for Neovascular Age-Related Macular Degeneration: Two-Year Results of the ANCHOR Study. Ophthalmology, 116(1).
[6] Schargus, M., & Frings, A. (2020). Issues with intravitreal administration of anti-vegf drugs. Clinical Ophthalmology, 14, 897–904.www.dovepress.com/
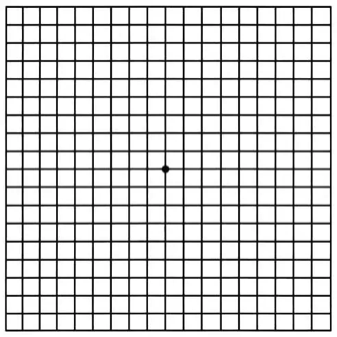
AMSLER GRID
Site by Constant Creations
Click here to return to Top of Page
Click here to return to Top of Page
Click here to return to Top of Page
Click here to return to Top of Page

